Abstract
The paper is devoted to a brief but nevertheless in-depth analysis of meaningful use of data in light of the HITECH Act of 2009. The findings clearly demonstrate the relevance of meaningful use of data along with existing gaps in the initial planning and implementation of the regulation. On the one hand, adherence to the set core criteria gave practitioners a possibility to improve their operations in a number of ways. Moreover, many providers have been using EHR in accordance with these criteria even before the regulation was enacted. On the other hand, the scope of information regarding patient-centered data entry is too limited to effectively impact the quality of care provided. Hence, a proposal to reconsider this aspect of meaningful data use was outlined in this regard.
Keywords: Meaningful Use, electronic health records, healthcare information exchange
Meaningful Use of Healthcare Data
This paper briefly reviews the Meaningful Use doctrine in order to identify and clarify possible gaps in the regulation and to propose some evidence-based solutions as a way of enhancing its practical efficacy. First, this essay focuses on an overview of the issue, its background, criteria, and intents. Second, the analysis of implications of the Meaningful Use core criteria follows. On the basis of the discussion, additional recommendations or their irrelevance are highlighted within the context of academic evidence. Finally, conclusions are drawn in light of the findings.
Overview of Meaningful Use
Place New Order
To start with, a concept of meaningful use is linked to the Health Information Technology for Economic and Clinical Health (HITECH) Act adopted in 2009 (Wright, Henkin, Feblowitz, McCoy, Bates, & Sittig, 2013). In accordance with this regulation, Medicare and Medicaid programs offer financial incentives to physicians and hospitals which incorporate electronic health records (EHRs) in the care provision operations in a sophisticated manner (Wright et al., 2013; Jha, 2010). The latter implies that these stakeholders should implement EHRs in a way that would facilitate higher quality healthcare services delivery and patient outcomes rather than simply organize a paradigm shift from the paper-based to electronic data reporting. In particular, this transition is grounded on directing this chance in light of improvement of patient care through efficient access to complete patient information (Estabrooks et al., p. 575).
Therefore, in order to achieve the set objective, meaningful use within healthcare facilities should correspond to a few core criteria which are summarized in Table 1 below. In general, the primary aspects to consider refer to entry of basic patient data, electronic prescribing, decision support, and the ability to perform health information exchange (Adler-Milstain, Bates & Jha, 2011, p. 666).
Table 1
Core criteria of meaningful use (Blumenthal & Tavenner, 2010, p. 502)
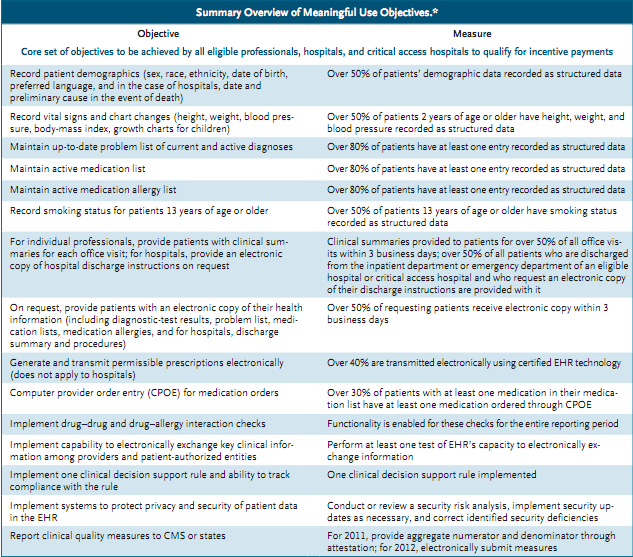
Apart from the abovementioned core criteria, a number of menu criteria were listed as optional perspectives that are worth taking into account for meaningful data use.
Analysis
First and foremost, digitalizing of healthcare-related data is a great way to incorporate a variety of different-character records in one place, for instance, a hospitals intranet system, and to ensure their authorized accessibility at any moment of necessity. Such an approach allows timely and efficient diagnosing of a patient, immediate interprofessional collaboration, instant review of the ones medical history, to list a few. Moreover, patients do not have to recollect their memories in terms of their previous health conditions and issues, since all the necessary records are already gathered and stored in an electronic healthcare recording (EHR) system. Collection of multidimensional patient-related data in such a way is a great approach to make a variety of treatment-based procedures easier for both parties.
Current healthcare system experiences a paradigm shift to growing complexity of activities performed today (Ventura et al. 163). In this light, availability of multifaceted patient-centered data which should be only retrieved from the place of their secured storage rather than collected anew allows a much quicker response to a patients concerns and needs. Furthermore, a part of EHR involves collection of the most up-to-date best practices and research findings structured according to different characteristics of healthcare system. For example, such data arrays may refer to symptoms of a particular disease, the most successful approaches to its treatment, medications to be prescribed in a specified case, and factors to be avoided, to name but a few.
Whereas incorporation of technology in hospital operations is based on the benefits of time efficiency, the issue of enhanced and instant communication within the context of multidimensional healthcare system should not be underestimated. Following the reasoning by Palma, medical professionals of different specialties or ranks can easily communicate with each other by means of an online-based EHR. This factor includes quick consultancy, practice details and experience exchange, scheduling of meetings in accordance with individual plans and aspirations or electronic notifications as well as cancelling of an appointment, if needed, among others. It follows that EHR can make the entire healthcare system more time-and-cost efficient and better planned.
- Our custom writing services includes:
- Plagiarism and AI free custom writing for the best grades;
- CV, resume and cover letters which would
make you successful - Thesis and dissertations writing by academic
authors
Similarly, a variety of professional communities, such as different organizations uniting healthcare practitioners by specialties, are Internet-mediated. Hence, an opportunity to share knowledge with one another and electronic exchange of experience can be developed not only inside a particular organization but also in a broader context of global cooperation. The data of this type can also be accumulated by a EHR system as an implication of both internal and external shared-knowledge framework aimed at advanced and high-quality care provision. As a result, staff members can explore the knowledge that is accessible online and exploit any time they need it for their working process.
Apart from that, EHR is favorable in light of professionals accountability. On the one hand, this factor implies development of an advanced system with relation to the hospitals medical equipment, staff that is involved in treatment and other activities, testing and other facility-centric resources as well as activities that are further billed to the patient (Palma). Thus, aggregation of such data enables smoothness and transparency of the patient-to-provider relationships. On the other hand, accountability can be regarded in the context of minimized ordering and drug or treatment prescription errors as contrasted to handwritten ones (Palma). To illustrate, a provider can immediately clarify availability of a particular drug in pharmacies. Additionally, typed recipes of drug prescriptions can be easily read by pharmacists without misinterpretation of the prescribed drugs because of bad calligraphy of a physician.
EHR can be a valuable instrument for screening and preventive health measures. As previously noted, EHR is a system incorporating huge amounts of multifaceted data regarding population as a whole. Further, the obtained information is segmented and classified. Thus, a physician has an opportunity to trace the state of health of specified groups of population in accordance with their health records, epidemics, threats to their health due to specific factors, such as a seasonal acute condition. For instance, a doctor can look through ones records stored in EHR system and identify the individuals classified with respect to belonging to, for example, an at-risk cancer patient group. If their time for a check-up visit has come or they should perform a specified diagnostic procedure, such as mammogram, a healthcare practitioner can notify them via e-mail and schedule an appointment for a consultation (Palma). Similarly, notifications for medical professionals may be scheduled in this respect as well.
Meaningful Use Recommendations
What are you waiting for?
Order with 15% discount NOW!

Based on the evidence from contemporary studies, the criteria proposed by the HITECH Act in terms of meaningful data use corresponded to the functions performed by physicians and healthcare practitioners who have referred to technology-mediated recording of data prior to the regulations implementation. Such findings relate to the study by Estabrooks et al. (2012) ascertaining that approximately 75-80 physicians and healthcare providers followed the set criteria before the regulation was developed. At the same time, the scholars have discovered a sufficient gap in setting the core criteria, which is a great shortcoming in policy efficiency and should be taken into account. To be more precise, the researchers have indicated a limited scope of mandatory entry of patient data covered in accordance with the identified criteria. As a result, Estabrooks et al. (2012) have referred to a necessity in updating and expanding the core-metrics framework as shown in Figure 1 below.
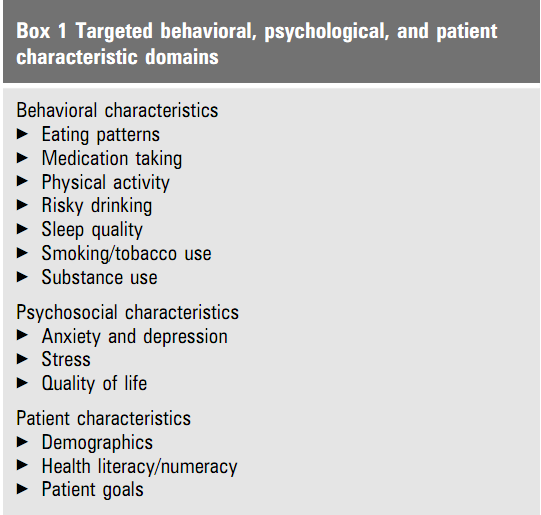
Figure 1. An updated core criteria framework (Estabrooks et al., 2012, p. 576)
Specifically, the issue refers to a broadened overview of patient psychological, behavioral and other health-related aspects of patients health records history. Indeed, all these factors greatly contribute to development and increased risks of chronic diseases in target population. Thus, these data can undermine the quality of care and healthcare information exchange in general. In contrast, relevance of this information and its up-to-datedness will grant the healthcare institutions an opportunity for smooth data-driven collaboration and increase in quality of care delivery.
Conclusion
The findings of the paper clearly demonstrated that incorporation of EHR in healthcare system as a standard procedure has both beneficial and disadvantageous aspects. On the one hand, numerous implications of EHR prove its multi-level efficiency for healthcare providers. The issue involves enhanced communication between practitioners, easy access to a variety of healthcare-specific theoretical and evidence-based data, smoother cooperation opportunities, to list a few. On the other hand, availability of consumer-sensitive data at one place presupposes an issue of its misuse and illegal activities. At the same time, dehumanization of this aspect of healthcare activities and constant supplementary funding and updating of the software and hardware packages become sufficient disadvantages of EHR. Nonetheless, thorough awareness about these issues will allow their eliminating at the planning stage.
